Enhancing Accuracy in First Injury Assessment Through Continuous Education
The primary goal of initial injury assessment is to understand the extent of the damage suffered and to ensure effective treatment can be administered. The initial assessment starts with gathering thorough history data about the injury occurrence, which helps medical professionals understand the context and mechanism of injury. This information can include details like how the injury occurred, the timing, and any immediate symptoms experienced. Health practitioners must also assess the vital signs and overall physical condition of the patient to identify critical or life-threatening issues. Evidence-based approaches advocate for the use of standardized assessment protocols that can minimize errors and improve patient outcomes. In addition, these protocols reinforce the importance of comprehensive training in initial assessments for healthcare providers. Regularly scheduled workshops, courses, and simulations can be key strategies in keeping knowledge current and ensuring practitioners are skilled in the latest assessment techniques. By pursuing ongoing education, professionals remain informed about new assessment methods and technologies that facilitate accurate evaluations. This approach not only enhances confidence among practitioners but also aids in building patient trust and satisfaction.
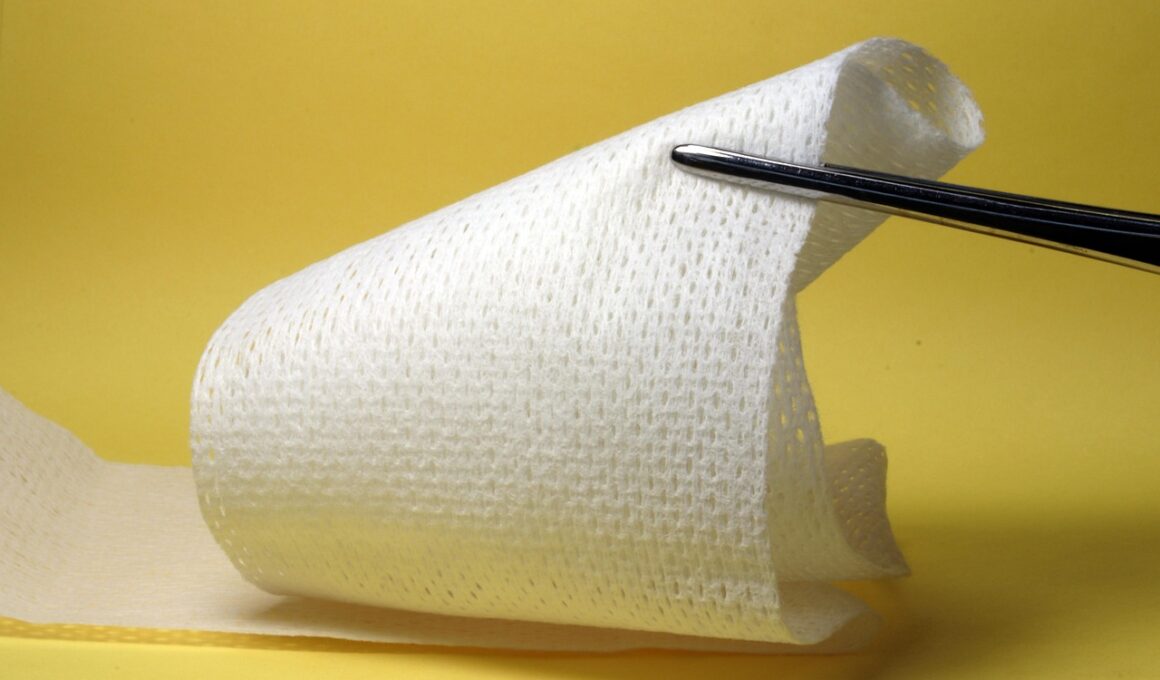
Moreover, utilizing effective communication skills during injury assessment is immensely vital for gathering the required data. Healthcare providers must ensure they actively listen to the patient’s account of their symptoms and injury context for precise evaluation. This process includes asking open-ended questions to encourage patients to describe their symptoms in detail, which can lead to better understanding and important insights about the injury’s severity. Listening carefully also helps build rapport, increasing the likelihood that patients will provide accurate and comprehensive information. Additionally, the skills developed in communication training can improve teamwork among healthcare providers, leading to more collaborative assessments. Moreover, assessments should include visual inspections and physical examinations while considering the patient’s pain levels and functional limitations. Using assessment tools, such as visual analog scales for pain, can support a more nuanced understanding of the situation. Collecting overall patient input effectively leads to the creation of tailored treatment plans aiming at fostering quicker recovery. Continuous education, in this context, plays a significant role in enhancing these communication techniques, allowing practitioners to adapt in various settings to diverse patient populations.
Importance of Hands-On Training
Hands-on training opportunities are indispensable for improving the skills associated with initial injury assessments. Participating in simulation-based experiences provides a realistic atmosphere for practitioners to acquire and practice assessment skills on dummy patients. This interactive approach helps mark critical assessment techniques and decision-making under simulated conditions similar to real-life scenarios. Furthermore, it allows practitioners to learn from their successes and mistakes in a safe environment, thus extending their knowledge base without patient risk. Continuous education programs that incorporate hands-on training help reinforce theoretical knowledge into practical applications, ensuring that skills are transferable. The goal is to build confidence among healthcare providers, diminishing the hesitation often associated with high-pressure situations. Moreover, ongoing assessments of learning outcomes from these programs provide analytics support to refine and improve training methods continuously. Encouraging peer feedback during simulation sessions can also enhance the practical learning experience for participants. Importantly, organizations should integrate hands-on skills assessments into training regularly to ensure that all personnel remain competent in their roles when faced with a variety of injuries, guaranteeing the best patient care.
Furthermore, standard operating procedures (SOPs) should be consistently revised to reflect the latest evidence-based practices for injury assessment. This alignment ensures that all healthcare professionals operate from a shared understanding of best practices and have ready access to the latest guidelines. Adopting updated protocols enhances the quality of patient care, minimizes errors, and ultimately improves the outcomes of initial assessments. For instance, implementing a checklist can help guide healthcare providers through the necessary assessment steps, ensuring none are overlooked. Additionally, integrating technological innovations like telehealth consultations can enhance initial assessments by enabling specialists to assist remotely. Training programs should also emphasize incorporating these technologies to ensure competency among healthcare professionals working in various environments. By fostering a culture of continuous improvement in practices, healthcare organizations can encourage their teams to stay abreast of updates within the medical field. Regularly updating SOPs serves as a crucial component of quality assurance, where protocols are shaped through acquired insights and real-world experiences by healthcare workers engaged in initial injury assessment.
Utilizing Feedback for Improvement
Another critical component of enhancing accuracy in initial injury assessment is actively seeking and utilizing feedback from peers and patients. Encouraging feedback helps identify areas that may require improvement, reinforcing the idea that education is an ongoing journey. Various channels can be established to streamline this feedback process, such as assessment feedback surveys or debriefing sessions post-training. Regularly gathering input from diverse sources creates a more profound understanding of common challenges faced during assessments. Furthermore, using feedback to develop targeted training modules allows organizations to address current knowledge gaps and adapt educational offerings to meet the needs of their staff effectively. For instance, if a particular assessment technique is frequently flagged by peers as challenging, targeted workshops can be organized to address these issues directly. Emphasizing a culture of constructive feedback fosters an atmosphere of shared responsibility among healthcare providers. Additionally, ongoing mentorship programs can help initiate conversations about performance and provide constructive avenues for improvement, which can ultimately lead to increased accuracy in injury assessments and, therefore, better patient care.
Moreover, technology is increasingly becoming an integral part of injury assessment, enhancing both accuracy and efficiency through various tools and applications. Digital platforms that offer injury databases can provide healthcare providers with access to a wealth of information regarding specific injuries, symptoms, and the latest treatment protocols. This access allows for informed decision-making during the assessment process, contributing to better clinical outcomes. Mobile applications designed explicitly for health practitioners can facilitate the documentation of assessments, which ensures the timely and accurate relay of critical data. These technologies allow for better tracking of patient history and streamed analyses of injury patterns, enhancing the overall understanding of injury dynamics. Furthermore, tools for image capturing, such as smartphones or tablets, can assist in visual assessments. Incorporating augmented reality (AR) technologies may also innovate how injuries are assessed by providing real-time visual context. Continuous education programs should include training on emerging technologies to equip healthcare professionals with the skills to utilize these advancements effectively and responsibly in their practice.
The Role of Multidisciplinary Collaboration
Lastly, fostering a multidisciplinary approach to injury assessment is imperative for achieving comprehensive evaluations. Collaboration between various healthcare professionals—physicians, physical therapists, athletic trainers, and other specialists—can lead to a holistic understanding of an injury. By integrating diverse perspectives, practitioners can create more effective and personalized treatment plans for each patient. Continuous education programs should reinforce the importance of teamwork, encouraging professionals to engage with colleagues from different disciplines. Interdisciplinary workshops and joint case studies can promote essential skills in collaborative techniques that enhance the accuracy of initial assessments. Such collaborations enable sharing of expertise while minimizing information gaps among team members. Additionally, regular team meetings allow individuals to discuss challenging cases and share successful assessment strategies. This collective wisdom leads to higher-quality patient care by ensuring that injuries are addressed from multiple angles, improving overall outcomes. Moreover, effective collaboration enhances communication skills among team members, as they emphasize listening and valuing each other’s contributions to injury assessment processes.
In conclusion, the pursuit of continuous education is vital for enhancing accuracy in the initial assessment of injuries. Maintaining up-to-date knowledge, honing practical skills, and adopting a collaborative approach can significantly impact patient care outcomes. The integration of technology, feedback mechanisms, and standardized protocols ensures effective assessments that minimize errors. Investing in education and training prepares healthcare providers to address the complexities of injuries, equipping them with the necessary tools and knowledge for making accurate assessments. Emphasizing hands-on learning experiences and multidisciplinary collaboration fosters well-rounded competencies in practitioners, enabling them to adapt to new challenges in diverse settings. Future directions in improving initial assessment methods involve ongoing evaluation and incorporation of advances in injury assessment technology. Consequently, a culture focused on continuous improvement resonates throughout healthcare settings, ultimately benefiting patients and health professionals. By instilling an attitude of lifelong learning, organizations can empower their teams and ensure unparalleled quality in care delivery. Embracing this culture will leverage enhanced patient trust and satisfaction, yielding positive feedback loops, thereby motivating further professional development and knowledge acquisition within the field.