Medication and Hydration: What Every Athlete Should Know
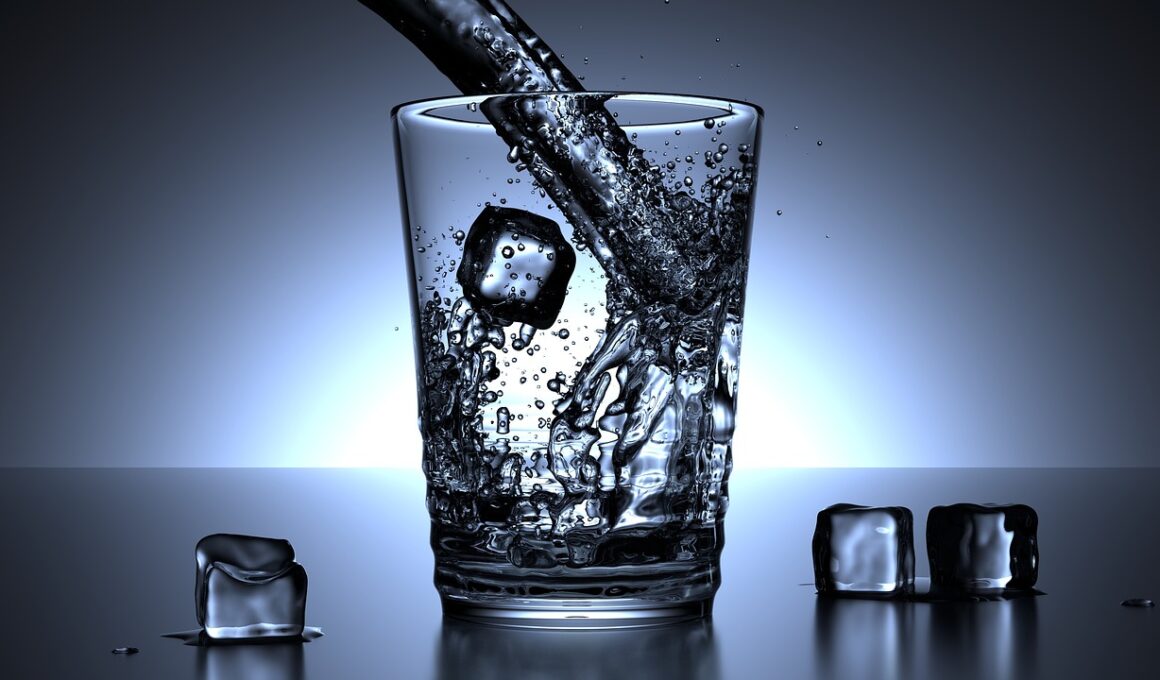
Hydration is crucial for athletic performance, but many athletes overlook hydration’s role in medication interactions. Understanding how medications influence hydration levels can significantly impact athletic performance and health. For example, certain diuretics can lead to excessive fluid loss, promoting dehydration symptoms such as fatigue or dizziness, which may impair athletic performance. Athletes taking medications should be aware of their hydration needs while also considering the combined effects of these substances. It’s vital to monitor fluid intake, especially during exercise. Athletes must consult with healthcare providers to adjust their hydration strategies as necessary. A personalized hydration plan encourages athletes to maintain fluid balance. Furthermore, hydration methods vary widely among different sports; thus, athletes should tailor their approaches based on their specific needs. Always remember that personal factors, including body weight, sweat rate, and environmental conditions, impact hydration and medication interactions during athletic activities. Being informed about these relationships can optimize athletic performance and maintain well-being. By prioritizing hydration management and medication awareness, athletes can enhance both their performance and their overall health.
Understanding Medication Effects on Hydration
Medications can have a variety of effects on hydration, some of which are more pronounced than others. Caffeine-containing medications, for instance, may act as mild diuretics leading to increased urine production. This can cause fluid deficit during exercise, particularly in endurance athletes engaging in prolonged activities. Understanding individual responses to medications is crucial for athletes aiming to optimize hydration strategies. Recommendations typically include increased fluid intake on days medications are taken regularly. Likewise, non-steroidal anti-inflammatory drugs (NSAIDs) can affect kidney function, potentially altering fluid balance in some individuals. Athletes should be aware that hydration requirements might differ when medications like these are introduced. Another commonly overlooked aspect is the impact on appetite; certain medications can decrease thirst sensations, making it essential for athletes to remain proactive about fluid intake. Regular hydration reminders, such as timers or hydration apps, can be quite beneficial. Overall, understanding how medications impact hydration is vital for athletes. Adapting hydration strategies while considering medications can maximize performance, endurance, and recovery. Knowledge of personal fluid needs, affected by specific medications, fosters better hydration practices.
Electrolyte Considerations in Hydration
Electrolyte levels can be significantly influenced by medication and hydration interplay, especially in athletes. Essential electrolytes like sodium, potassium, magnesium, and calcium play crucial roles in muscle function and performance. Dehydration often leads to an imbalance of these electrolytes, which can adversely affect an athlete’s performance capability. Athletes on diuretics, for instance, risk experiencing severe electrolyte imbalances as these medications promote fluid loss. To combat these potential pitfalls, athletes should consider replenishing electrolytes lost during intense training sessions. Sports drinks available on the market can help restore these essential minerals quickly, ensuring athletes maintain optimal performance. Additionally, dietary adjustments may be necessary to increase electrolyte-rich foods in an athlete’s nutrition plan. Foods such as bananas, oranges, and leafy greens provide significant potassium and magnesium. Hydration strategies that incorporate electrolyte replenishment can enhance recovery after strenuous exercise and reduce muscle cramping. Timely restoration of these crucial compounds is thus paramount for athletes, especially during competition. Always consult with a healthcare provider for tailored hydration strategies and dietary recommendations concerning medications. Proper electrolyte management ensures athletes remain at peak performance levels.
Fluid absorption rates can vary significantly based on the type of hydration strategy implemented. Athletes need to consider how medications may influence these rates and, consequently, their recovery and performance. For example, certain medications may impair gastric emptying, which hinders optimal fluid absorption during strenuous activities. Timing hydration before, during, and after competition is critical to ensure peak fluid intake aligns with absorption rates. Additionally, the consumption of high-sugar drinks may lead to gastrointestinal discomfort, further complicating hydration strategies. Athletes should evaluate the types of beverages they consume after taking medications that might interfere with bodily functions. Choosing beverages designed for faster absorption, such as electrolyte solutions, can significantly aid hydration efforts. Furthermore, maintaining consistent hydration habits during training can help develop an athlete’s personalized hydration strategy that meets their demands regardless of medication use. Experimenting during training sessions is key to finding optimal hydration methods. Incorporating these strategies ultimately fosters more effective hydration, better performance, and faster recovery. Athletes must prioritize hydration knowledge while managing medications for better health outcomes.
Tailoring Hydration Strategies
Individualized hydration strategies are essential for athletes, especially when taking medications that influence hydration needs. Factors such as body type, age, sex, local climate, and duration of exercise can dictate an athlete’s optimal hydration plan. Incorporating personalized hydration options can maximize results, ensuring that every athlete maintains an adequate fluid balance. Athletes should actively monitor body weight before and after workouts to gauge fluid loss and adjust fluid intake accordingly. Fluid intake recommendations generally suggest 500 mL of water per hour as a baseline, but this may be modified based on medication side effects. For instance, an athlete on diuretics may require more frequent hydration breaks during training sessions. Additionally, incorporating flavorful beverages can help encourage hydration by enhancing palatability. Water is essential, but experimenting with alternatives such as coconut water or electrolyte-rich drinks may yield better results. Comprehensive education on hydration strategies can empower athletes to make informed choices, further promoting successful hydration practices. Customizing these strategies can lead to optimal physical performance while minimizing the side effects of medications that might impair fluid balance.
Staying Informed: The Athlete’s Advantage
Being informed about the types of medications being taken is essential for athletes to optimize hydration strategies effectively. This awareness allows athletes to discuss any concerns relating to hydration and medications with healthcare professionals, creating a proactive approach to health management. Athletes should regularly update coaches and trainers on any medications being prescribed, as this enables adaptations in training regimens that consider hydration specifics. Continuous education on the medication’s effects on hydration and performance also contributes to enhancing overall wellness. Utilizing available resources, such as workshops or webinars focused on medication-hydration interactions, can bridge the knowledge gap in this area. Furthermore, engaging in discussions with fellow athletes and nutritionists may provide valuable insights to improve personal hydration strategies. Information technology, including apps and hydration tracking programs, can facilitate better management of fluid needs. Staying up-to-date with research findings on hydration guidelines and medication interactions empowers athletes to make data-driven decisions. Ultimately, enhancing hydration literacy amid medication use allows athletes to sustain peak performance while ensuring their health is prioritized during training and competitions.
In conclusion, effective hydration strategies are paramount for every athlete, especially those taking medications that affect fluid balance. The interplay between medications and hydration is complex and must be navigated carefully. Athletes should adopt personalized hydration plans, considering medication effects, individual needs, and electrolyte balance. Staying informed through continuous education and consultations with healthcare providers can significantly improve hydration management. By doing so, athletes not only enhance performance but also support overall well-being. Proactive hydration management creates synergy between medication use and athletic activity, ultimately leading to the achievement of athletic goals while preserving health. Commitment to hydration education and practice should be a top priority for all athletes. Efforts to investigate and integrate evidence-based hydration strategies into training regimens will empower athletes to achieve optimal performance outcomes. Aligning hydration practices with the nuances of medication effects further facilitates better health management. Whether training for the next competition or maintaining daily fitness, understanding hydration’s critical role in conjunction with medication use is essential. Athletes should embrace these strategies to maintain endurance, foster recovery, and ensure healthy hydration practices.
Since athletes typically have unique hydration challenges, understanding medication interactions can provide a significant advantage. In-depth evaluation and ongoing assessment of hydration strategies can further refine practices as athletes respond to medication changes or personal performance variables. Emphasizing the importance of proper hydration and awareness about medication interactions can pave the way to improved athletic success. Knowledge is power, and well-informed athletes are more likely to reap the benefits of their hard work and training. Recommendations may include conducting hydration workshops within teams to exchange information and strategies. Regular team discussions about medication effects on hydration can motivate collective effort towards optimal hydration practices that support performance and health. Coaches can play a vital role by encouraging diligent hydration habits and fostering an open environment where athletes feel comfortable discussing medication-related concerns. Effective collaboration among athletes, coaches, and medical professionals is crucial to achieve an all-encompassing hydration approach. Ultimately, implementing comprehensive hydration strategies does not only affect performance outcomes but also promotes overall health. Continuous attention to hydration management will serve as a valuable investment for aspiring athletes.