Cardiac Remodeling in Response to Regular Exercise
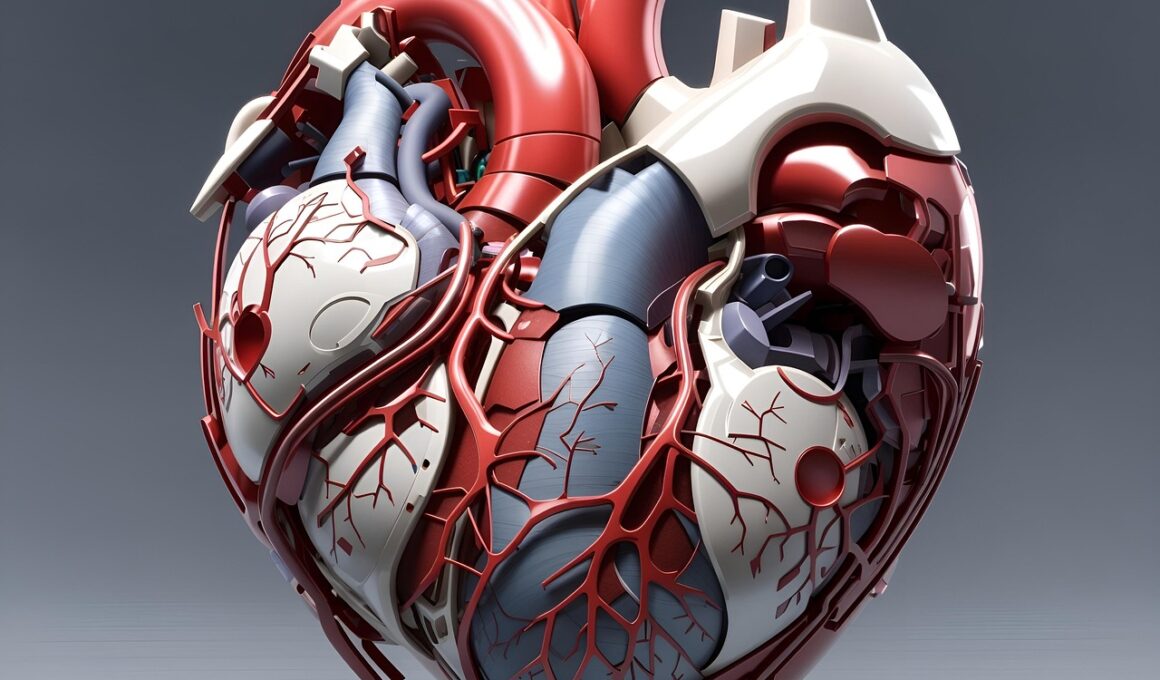
Cardiac remodeling is a vital adaptation process that the heart undergoes in response to regular exercise. This process enhances cardiac function and improves overall cardiovascular health. There’s substantial evidence that regular physical activity leads to beneficial changes within the heart, such as increased wall thickness and enhanced chamber size. Exercise-induced cardiac remodeling consists of both structural and functional changes. Structural changes often include hypertrophy of the myocardium, which helps the heart pump blood more efficiently during exertion. Conversely, functional adaptations might encompass improved cardiac output and increased stroke volume. Understanding how exercise affects the heart at these levels can guide professionals in recommending appropriate activities for athletes and patients alike. Regular exercise substantially mitigates cardiovascular diseases; it reduces hypertension, hyperlipidemia, and enhances insulin sensitivity. On an individual level, people who partake in consistent aerobic exercise often report improved quality of life. However, it’s essential to note that excessive exercise without adequate rest can lead to negative adaptations, and individuals should be educated on balancing activity and recovery. Overall, the cardiac remodeling process is critical in adapting the heart to the demands placed on it during regular physical activity.
The physiological mechanisms underlying cardiac remodeling are multifaceted and intricately linked to exercise intensity and duration. When individuals engage in regular aerobic or resistance training, the cardiac muscle cells respond by hypertrophying. This process occurs due to the mechanical stress exerted on the heart, which stimulates the release of growth factors and hormones such as norepinephrine, adrenaline, and atrial natriuretic peptide. These factors play a crucial role in mediating the remodeling processes by promoting myocardial growth and altering gene expression. Additionally, cardiovascular adaptations arise through improved angiogenesis, which is the formation of new blood vessels. Increased blood vessel density optimizes blood supply to the heart muscle, thereby enhancing oxygen delivery during elevated physical exertion. Such adaptations collectively counteract the risk of ischemic heart disease. Notably, the remodeling response is influenced by genetic predispositions, age, and pre-existing health conditions. Therefore, personalized exercise regimens can enhance the efficacy of these adaptations. Monitoring and adjusting exercise programs ensures individuals achieve the maximum benefit while minimizing the risk of adverse outcomes associated with excessive physical stress.
Cardiac Adaptations to Exercise Training
Cardiac adaptations resulting from exercise training vary according to the type and duration of the exercise performed. Aerobic exercise, characterized by continuous, rhythmic activities such as running or cycling, leads to significant changes in heart structure and function. One of the primary adaptations is an increase in left ventricular size, which translates to enhanced stroke volume. This adaptation allows the heart to pump more blood with each contraction, reducing the overall heart rate required during physical exertion. Resistance training, on the other hand, promotes a different set of changes, primarily hypertrophy of the myocardium without a significant increase in cavity size. This adaptation helps in improving the heart’s pumping ability when lifting heavy weights. Interestingly, studies have shown that a combination of aerobic and resistance training yields the best overall cardiovascular benefits. Furthermore, regular exercise improves autonomic regulation of the heart. Enhanced vagal tone and reduced sympathetic drive contribute to this autonomic balance, promoting cardiovascular stability and efficiency. Therefore, incorporating varied forms of exercise offers unique benefits, leading to optimal heart health and effective management of cardiovascular conditions.
In addition to structural and functional adaptations, exercise plays a crucial role in cellular and molecular signaling pathways linked to cardiac remodeling. The process begins with the activation of various signaling cascades triggered by mechanical stress and hormonal stimulation during exercise. For instance, the phosphatidylinositol 3-kinase (PI3K) and mitogen-activated protein kinase (MAPK) pathways are pivotal in initiating the cardiac hypertrophic response. Moreover, the expression of certain genes involved in muscle growth and metabolism significantly increases with regular exercise. These molecular changes help to reinforce the heart’s ability to cope with increased demand. Additionally, exercise enhances the heart’s antioxidant defenses, reducing oxidative stress, a key factor in the development of cardiovascular diseases. The overall physiological benefits are complemented by improvements in endothelial function, which is vital for maintaining vascular health. Active individuals demonstrate better nitric oxide availability, promoting vasodilation and lowering systemic vascular resistance. Therefore, understanding the underlying mechanisms of cardiac remodeling enables healthcare professionals to advocate for exercise as a strategy for preventing and managing cardiovascular diseases effectively.
Effects of Exercise Intensity on Cardiac Remodeling
The intensity and frequency of exercise have a profound impact on the extent of cardiac adaptations. Research demonstrates that higher intensity workouts lead to more significant cardiovascular adaptations when compared to moderate exercise. High-intensity interval training (HIIT) has gained popularity due to its efficiency in improving cardiorespiratory fitness and promoting greater left ventricular hypertrophy. This type of training challenges the heart more effectively, thus optimizing remodeling changes. Importantly, individuals need to apply caution because excessive high-intensity training without adequate recovery can lead to negative adaptations, sometimes referred to as overtraining syndrome. This condition can place undue stress on the heart and result in impaired performance. In contrast, moderate-intensity continuous exercise, such as brisk walking or cycling, still offers substantial cardiovascular benefits without the risks associated with high-intensity training. For many individuals, a blend of intensities within a balanced fitness regimen can promote optimal adaptations while ensuring safety. Health professionals can utilize this knowledge to customize exercise programs tailored to individual fitness levels, maximizing the potential for positive cardiac remodeling.
While the benefits of cardiac remodeling due to exercise are well documented, it is vital to recognize individual differences in response to exercise. Genetic factors, age, and pre-existing conditions significantly influence how the heart adapts. For example, older adults might experience less pronounced cardiac remodeling compared to younger individuals due to age-related physiological changes. Similarly, individuals with cardiovascular diseases may require specialized approaches to exercise, as their hearts might respond differently to physical stress. Personalizing exercise programs involves assessing patient history and physical condition before developing a suitable regimen. Tailored training can also help mitigate injury risks while optimizing cardiac benefits. Furthermore, education about the signs of overtraining and maintaining a balanced approach to fitness is crucial for long-term adherence. Encouraging patients to monitor their responses to exercise can ensure they reap the full rewards while also promoting a lifelong commitment to regular activity. Developing fitness programs that align with individual goals and limitations will ultimately lead to improved health outcomes. Ensuring regular follow-up and adjustments will support their continued progress while fostering positive lifestyle changes.
The Role of Recovery in Cardiac Remodeling
Recovery is an essential aspect of the exercise regimen that directly influences cardiac remodeling and overall fitness. It is during recovery that the body repairs and strengthens tissues, including heart muscle, following the stress of physical activity. Inadequate recovery can lead to chronic fatigue, diminished performance, and potential cardiovascular issues. Periods of rest provide vital opportunities for regenerative processes, enabling optimal structural and functional adaptations to occur. Active recovery strategies, such as light exercise or mindfulness practices, can enhance recovery by promoting blood flow and reducing muscle soreness. Moreover, emphasizing adequate sleep and nutrition is critical to support the remodeling processes induced by exercise. Sufficient calorie intake, particularly from nutrient-dense foods, is essential for the rebuilding of cardiac tissues and optimizing energy availability. Additionally, hydration strategies play a role in cardiovascular performance and recovery. Therefore, successful fitness programs must incorporate structured recovery periods, ensuring that individuals do not overlook this crucial component. Coaching clients to balance activity with allotted rest times will contribute positively to their performance outcomes and diminish injury risk, fostering a healthier, more sustainable approach to fitness.