Emerging Trends in Exercise Physiology Research Related to Metabolic Diseases
The field of exercise physiology has seen significant advancements in the understanding of metabolic diseases, creating new pathways for research. Researchers now focus on how tailored exercise programs can help manage conditions such as obesity, type 2 diabetes, and metabolic syndrome. There is particular interest in the interplay between exercise intensity and various metabolic pathways that influence disease outcomes. Studies reveal that not only duration but also the type of exercise plays a critical role in improving metabolic health. High-Intensity Interval Training (HIIT) is being increasingly explored for its effectiveness in promoting fat oxidation while improving insulin sensitivity. Fat loss coupled with improved metabolic function highlights why exercise is an essential component in the management of metabolic diseases. Moreover, ongoing research emphasizes the importance of individualizing exercise prescriptions to match personal health profiles and preferences. The incorporation of technology, such as wearables and mobile health apps, provides real-time data, making it easier for individuals to engage in and monitor their exercise habits. Scientists are now recommending periodic assessments to adapt exercise regimes effectively as Metabolic Diseases often present diverse challenges.
Innovative Approaches in Exercise Recommendations
Recent studies have suggested innovative approaches to exercise recommendations for individuals with metabolic diseases. Interdisciplinary collaborations among exercise physiologists, nutritionists, and healthcare providers enhance the development of comprehensive treatment plans. Exercise prescriptions are now becoming more dynamic, focusing on progression over time rather than static recommendations. Specific attention is paid to monitoring physiological responses during exercise, making adjustments as patients adapt to increasing workloads. Emerging technologies like telehealth are facilitating greater access to expert guidance, ensuring tailored fitness programs align with each individual’s needs. This leads to improving adherence rates considerably among patients facing metabolic disorders. Research indicates that small, incremental changes can lead to significant health improvements, therefore promoting sustainable lifestyle modifications. Additionally, mental and emotional well-being is explored by implementing exercise routines that foster social connections, making exercise a community-oriented activity. Employing motivational strategies within regimes can further enhance participant engagement, ultimately improving metabolic health outcomes. With these innovative methodologies, the most recent trends indicate that addressing the psychological aspects of exercise is just as crucial as the physical components, forming a well-rounded strategy in exercise physiology.
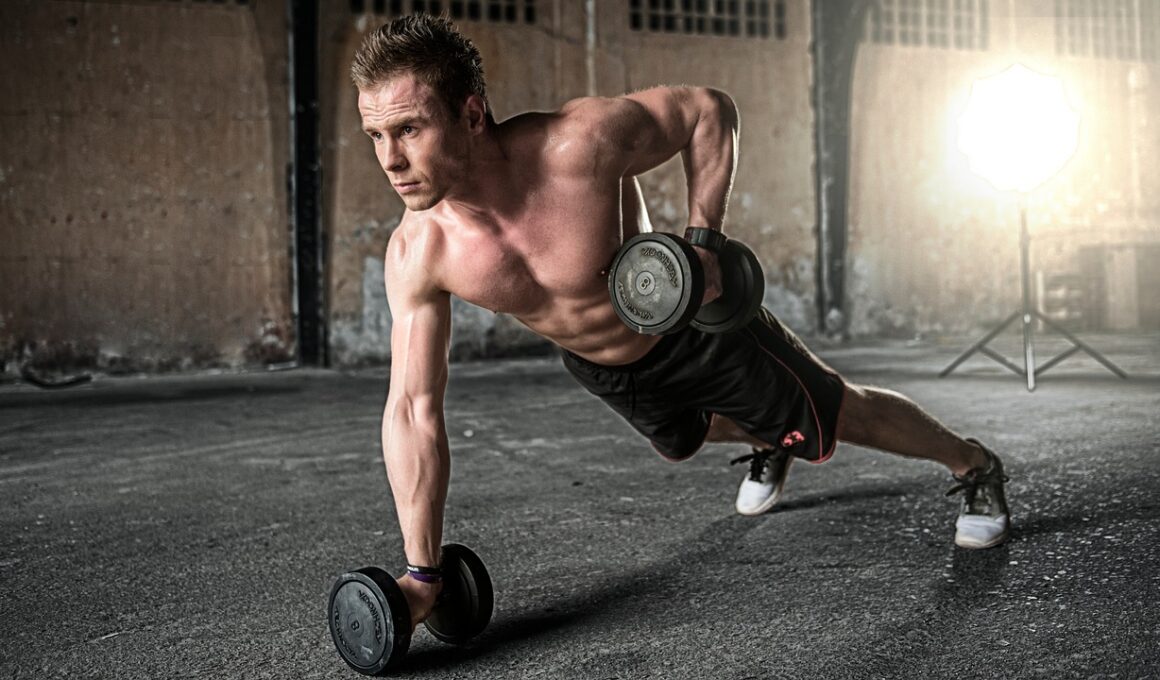
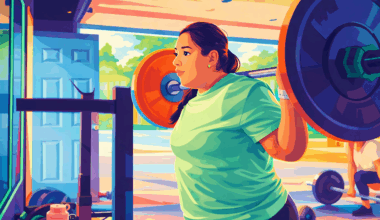
The role of resistance training within exercise physiology continues to gain traction in combating metabolic diseases. Evidence supports that strength training not only builds muscle mass but significantly improves metabolic health, especially among older adults. By enhancing muscle insulin sensitivity and glucose uptake, resistance exercises can have a profound effect on managing conditions like diabetes and obesity. Moreover, integrating resistance training can lead to favorable body composition changes, ultimately reducing obesity-related complications. Current trends illustrate a shift towards acknowledging how muscle quality and quantity impact longstanding metabolic health. Emphasizing the need for incorporating resistance exercises into regular fitness routines, healthcare professionals are now advocating for a combined approach with aerobic exercises to optimize outcomes. Increased focus on lifestyle coaching has also emerged, supporting individuals in integrating resistance training into their daily lives. This integration can be particularly beneficial given that many patients may feel intimidated by traditional physical activity guidelines. Researchers continue to analyze the effectiveness of community-based programs that promote fun and engaging resistance activities. Finding exercises appealing encourages participation and fosters resilience, thus improving patients’ overall metabolic health long-term.
The Importance of Personalized Exercise Regimens
Personalized exercise regimens emerge as a cornerstone in the fight against metabolic diseases. Instead of one-size-fits-all approaches, researchers are uncovering the value of customizing exercise plans based on individual genetic profiles, lifestyle habits, and personal preference. This tailored methodology can enhance the effectiveness of interventions aimed at treating and preventing metabolic disorders. Many recent studies indicate that air quality, local environments, and familial support greatly influence exercise adherence and overall health outcomes. Utilizing genetic information can identify potential responses to different forms of exercise and dietary regimes, allowing healthcare specialists to create optimal fitness plans. As more people seek personalized plans, the integration of data analytics with wearable technology provides new opportunities for tracking progress and adjusting workout routines. Furthermore, the development of community-based fitness initiatives focused on individuals with similar metabolic challenges has shown promise in generating positive results. These programs help participants foster connections, share experiences, and promote security among peers. The continued exploration of personalized regimens signifies a more refined approach in exercise physiology, catering to the unique needs of individuals with metabolic diseases.
Emerging research continues to highlight the role of continuous monitoring in the realm of exercise physiology and metabolic disease management. Real-time monitoring through wearable devices provides invaluable data on heart rates, step counts, and energy expenditure. This information empowers both healthcare providers and patients to fine-tune their exercise plans based on current physiological responses. Individuals can track their progress towards set goals, promoting better motivation and accountability. As smart technology evolves, researchers are investigating the impact of biofeedback on exercise performance, enhancing individual understanding of how their bodies respond to different routines. The integration of artificial intelligence into these technologies potentially opens doors toward predicting individual responsiveness to exercise. With such advancements, both adherence to exercise motors and achieved outcomes in treating metabolic diseases could see substantial improvements. Furthermore, ongoing studies aim to understand how personal preferences in technology influence engagement levels with exercise routines. This narrative signifies a changing landscape, where continual feedback loops create more informed and adaptable routines for individuals experiencing metabolic diseases, allowing for holistic management of their conditions.
Emotional and Psychological Aspects of Exercise
Emphasizing the emotional and psychological aspects of exercise is critical in metabolic disease management. Research is increasingly showing that regular physical activity can combat depressive symptoms commonly associated with metabolic conditions. This holistic perspective is responsible for a paradigm shift in the way exercise physiology approaches treatment. Creating supportive environments for individuals can significantly influence their motivation to engage in regular exercise. The promotion of mindfulness within exercise routines has emerged as an effective strategy, allowing individuals to focus on their bodies’ responses while engaging in activities. Programs that integrate counseling or group support sessions alongside exercise have shown enhanced outcomes. Understanding the relationship between mental health and physical activity underscores the need for multi-faceted approaches in delivering exercise programs. Adopting motivational interviewing techniques can foster a positive environment for participants, leading to greater persistence in exercise routines. Current trends suggest that mental resilience plays a substantial role in achieving fitness goals, particularly in those with metabolic diseases. As continuities between mental and physical health become clearer, the need for comprehensive treatment strategies that bridge the gap is imperative for tackling this public health concern.
In summary, the landscape of exercise physiology as it relates to metabolic diseases is rapidly evolving. The integration of innovative practices, personalized approaches, and the emphasis on psychological well-being marks a new era in managing these complex health conditions. As researchers continue to explore the efficacy of different exercise types and intensities on various populations, the potential for improved health outcomes increases. Harnessing technology while maintaining a personal touch emphasizes the connections between patients and their exercise experiences. Social support systems are emerging as invaluable resources, enhancing motivation and adherence among participants. Additionally, educators and healthcare providers are undergoing training to understand better the nuances of emerging trends in exercise physiology research. The intricate relationship between exercise and metabolic health advances our understanding of lifestyle modifications necessary for prevention. Collaboration among professionals in various fields is critical to crafting effective strategies that encapsulate the entire spectrum of health. This comprehensive approach not only promotes physical fitness but also instills a sense of belonging and support, vital in maintaining long-term health and well-being for individuals affected by metabolic diseases.
The exploration of dietary interventions combined with exercise is becoming insatiably crucial in addressing metabolic diseases. Evidence suggests that nutritional strategies employed alongside exercise can yield transformative results on long-term health. Studies examining diet patterns, such as the Mediterranean and ketogenic diets, in conjunction with regular physical activity, reveal profound enhancements in metabolic outcomes. This synergy not only aids in weight control but significantly contributes to improved cardiovascular health as well. Collaborative research indicates how integrated approaches involving dietitian consultations alongside tailored exercise programs facilitate greater health engagement and adherence among patients. This narrative enables healthcare providers to emphasize a more holistic strategy that encompasses both physical activity and nutrition. Monitoring dietary adherence while individuals exercise promotes accountability and a deeper understanding of how foods impact metabolic states. Additionally, participants report enhanced experiences when they engage in group dietary sessions paired with fitness workouts, exemplifying the social components of lifestyle changes. Further investigations delve into the cultural factors that influence dietary choices and assess their implications on exercise effectiveness. The focus on comprehensive health models illustrates a potentially transformative direction in combating metabolic diseases through combined lifestyle modifications.