Body Composition and its Role in Gestational Diabetes Management
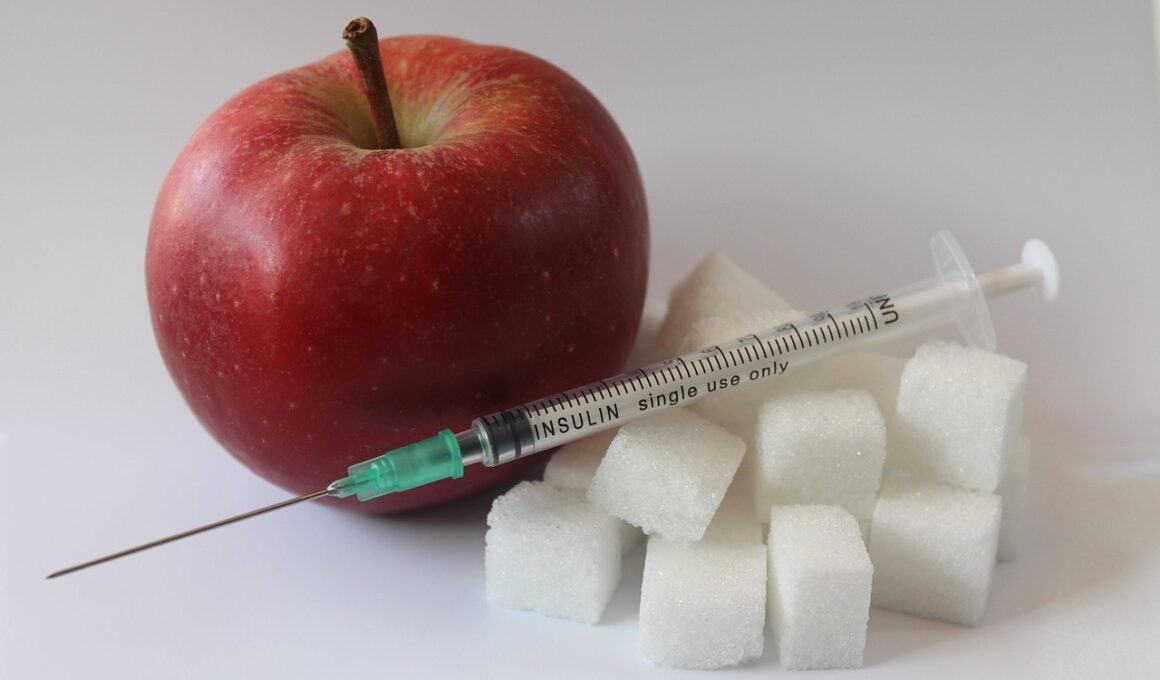
Gestational diabetes is a condition that affects women during pregnancy, characterized by high blood sugar levels. Understanding body composition is essential for managing this condition effectively. Body composition analysis helps identify fat and lean mass percentages, providing insights into a woman’s overall health during pregnancy. Maintaining a healthy body composition can significantly reduce the risk of gestational diabetes development and complications. Women with high body fat percentages are at an elevated risk of developing insulin resistance, a precursor to gestational diabetes. Strategies that promote healthy weight management and body composition improvements should be prioritized. Regular physical activity is vital in this process; it can help women achieve optimal body composition by reducing excess fat and enhancing lean muscle mass. Nutrition also plays a critical role—eating a balanced diet with adequate protein and healthy fats can aid in achieving better body composition. Healthcare providers should prioritize educating pregnant women on the importance of body composition for gestational diabetes management to ensure healthier pregnancies. This approach can foster better health outcomes for both mothers and their children, shedding light on body composition’s impactful role in pregnancy.
Body composition measurement techniques such as dual-energy X-ray absorptiometry (DXA) are invaluable for pregnant women. These methods provide precise insights into fat mass, lean mass, and bone density. Accurate measurements allow healthcare professionals to tailor approaches for managing gestational diabetes effectively. Moreover, body composition assessment may serve as a predictive tool, alerting healthcare providers to potential risks. A study indicated that women with higher body fat levels often experience difficulties in glucose regulation, amplifying the risk of gestational diabetes. Hence, ongoing monitoring of body composition throughout pregnancy is essential for early intervention. Prenatal care should incorporate discussions about body composition, emphasizing the relationship between excess body fat and insulin sensitivity. Educating women about maintaining healthy composition can empower them to make informed lifestyle choices. Consider developments in telehealth and digital tools, which may enhance access to coaching on weight, nutrition, and exercise. Additionally, interventions that focus on promoting sustainable weight loss before conception can dramatically improve gestational outcomes. It’s imperative to carefully evaluate various diet plans and exercise regimes and tailor them to individual needs. The goal is to optimize body composition, offering better insulin sensitivity.
The Importance of Nutritional Changes
Proper nutrition is paramount for managing body composition and gestational diabetes. A well-balanced diet rich in whole grains, lean proteins, vegetables, and healthy fats fosters better health during pregnancy. Such dietary habits can enhance women’s metabolic health and facilitate healthy weight gain. Interestingly, dietary fiber can significantly impact blood sugar fluctuations. Foods high in fiber can help slow down glucose absorption, stabilizing blood sugar levels. Studies emphasize the beneficial outcomes of adopting a high-fiber diet for pregnant women at risk of diabetes. Reducing refined carbohydrates and sugary snacks is crucial in mitigating insulin resistance. Additionally, regular meals and snacks can help stabilize energy levels while preventing significant hunger episodes. Educating women about mindful eating practices is beneficial, as it encourages them to pay attention to hunger cues and avoid overeating. This encourages a healthier relationship with food, which can lead to better body composition outcomes. Integrating nutritional education into prenatal programs can demystify healthy eating and make it more accessible. Encouraging supportive social networks can also facilitate healthier eating patterns, providing a community for shared experiences and encouragement during pregnancy.
A holistic approach to gestational diabetes management should involve both physical and emotional well-being. Stress management and mental health play significant roles in body composition and overall pregnancy health. Elevated stress levels can lead to unhealthy eating habits and poor lifestyle choices, which can adversely affect body composition. Techniques such as mindfulness, yoga, and deep breathing can be beneficial in managing stress. Supporting pregnant women emotionally through counseling and group support sessions can mitigate anxiety and promote healthier lifestyle adaptations. Furthermore, regular physical activity tailored to a woman’s physical capabilities is essential in managing body composition. Safe exercises during pregnancy can only improve body composition but also alleviate symptoms of pregnancy discomfort and boost mental health. Prioritizing milestones, small achievements, and recognizing improvement on body composition can encourage continued progress. Furthermore, healthcare providers can be instrumental in reinforcing positive behaviors and offering practical tips for integrating wellness routines into daily life. Regular follow-ups and personalized care can contribute significantly to improved health outcomes. Women must be equipped with the tools and resources to make informed decisions regarding their body composition management during pregnancy.
Physical Activity Recommendations
Physical activity during pregnancy can significantly impact body composition and energy levels. Engaging in regular exercise helps regulate blood sugar levels, promoting better glucose management for pregnant women. Even moderate activities, such as walking or swimming, can yield positive results. The ACOG recommends at least 150 minutes of moderate-intensity aerobic activity each week for pregnant women. Strength training, when performed safely, can also enhance muscle mass and improve metabolic rate. It is essential to engage in workouts tailored to pregnant women, focusing on activities that enhance core and lower body strength. This not only helps with weight management but also prepares the body for labor and delivery. Additionally, group classes or partner workouts can foster motivation and accountability. Pregnant women should listen to their bodies and adjust their routines according to comfort levels, ensuring safety at every stage. Staying hydrated and monitoring heart rate during workouts are essential considerations for maintaining health. Discussing perceived exertion levels with a healthcare provider can help in adjusting exercise intensity. A structured exercise plan can lead to optimal body composition, ultimately improving the management of gestational diabetes.
Technology is increasingly playing a vital role in monitoring body composition and managing gestational diabetes. Wearable devices and apps provide real-time feedback on physical activity, nutrition, and other health metrics. Such technology empowers women by encouraging self-monitoring and fostering accountability. Furthermore, trending blood sugar monitoring devices can allow for real-time insights, enabling women to manage their glucose levels effectively. This proactive approach helps in making healthier choices impacting body composition. Many apps also offer personalized meal planning and educational resources geared towards pregnancy. Women can benefit immensely from using these tools to receive tailored guidance focused on maintaining healthy body composition throughout pregnancy. Engaging with online health communities can also encourage sharing experiences and tips, leading to a supportive network. Telehealth consults can provide access to dietitians and personal trainers specializing in prenatal health, adding further value for women seeking tailored solutions. As technology evolves, the ability to personalize dietary and activity suggestions becomes more convenient and accessible. Holistic management encompassing lifestyle, body composition monitoring, backed by technology, can redefine gestational diabetes management practices.
Conclusion
In conclusion, managing body composition plays a fundamental role in dealing with gestational diabetes. A multifaceted approach integrating education, nutrition, physical activity, and emotional support can significantly contribute to healthier pregnancies. Encouraging regular body composition assessments allows for early adjustments to management plans, ensuring women receive tailored care. By emphasizing optimal body composition, pregnant women can accomplish better insulin sensitivity and mitigate the risk of gestational diabetes complications. Healthcare providers must prioritize this approach by offering comprehensive care focused on lifestyle improvements. Support systems, including family and community engagement, can further enhance overall outcomes. As research continues to uncover connections between body composition and health, incorporating these practices into prenatal care will be crucial. By taking proactive steps, women can ensure their well-being, ultimately leading to a healthier future for both themselves and their babies. The ongoing integration of modern technology in monitoring, along with sustainable practices, will aid in achieving these goals. Ultimately, empowering women through education and support can lead to profound improvements in pregnancy health and body composition management.
Acknowledging the importance of body composition is pivotal in gestational diabetes management. Future research should explore effective strategies to improve educational resources further. Exploring diverse dietary plans tailored to individual needs may also prove valuable in enhancing management practices. By focusing on holistic health, we can substantially improve outcomes for women facing gestational diabetes.