Understanding Body Composition Analysis for Diabetes Management
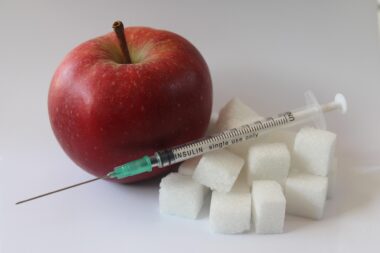
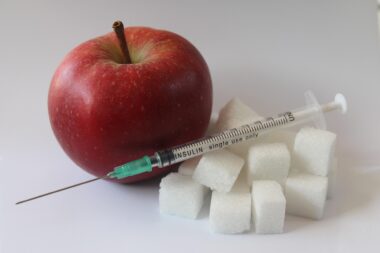
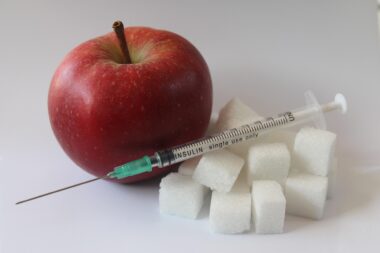
Body composition analysis is a crucial aspect of diabetes management, offering insights into a patient’s overall health. This analysis involves measuring the different components of body mass, including fat mass, muscle mass, and water content. In individuals with diabetes, understanding these components can lead to more personalized and effective treatment plans. By assessing body composition, healthcare providers can identify excess fat or unrecognized muscle loss, both of which are significant indicators in diabetes management. For example, an increase in visceral fat can signal a higher risk for insulin resistance. Moreover, tracking changes in body composition over time allows for the evaluation of health interventions. As a result, tailored exercises and dietary plans can be designed to optimize glucose management. Innovative tools such as bioelectrical impedance analysis (BIA) or dual-energy X-ray absorptiometry (DEXA) are often used for this purpose, helping to provide accurate measurements. These methods can help patients and doctors understand the impact of lifestyle choices on health outcomes, enhancing awareness about maintaining healthy body composition. Engaging in this analytical approach fosters a proactive stance in managing diabetes effectively.
One significant advantage of body composition analysis is its ability to identify specific fat distribution patterns. This insight is essential for developing targeted dietary and exercise interventions tailored to individual patients. Fat distribution is often classified into two types: subcutaneous fat located just beneath the skin and visceral fat surrounding internal organs. In diabetes, excessive visceral fat is particularly concerning as it contributes to metabolic disturbances and insulin resistance. Health professionals can utilize this information to encourage lifestyle modifications. For instance, patients may be guided to engage in regular aerobic exercises and strength training to decrease visceral fat levels. Additionally, dietary recommendations can be fine-tuned to promote fat loss while preserving lean muscle mass. Such personalized strategies empower individuals with diabetes to take control of their health actively. Regular follow-ups with body composition measures can also provide motivation, as patients witness progress over time. Furthermore, incorporating technology for carrying out body composition assessments ensures that the results are accurate, enabling real-time adjustments in management plans. Overall, the analysis is an invaluable tool not only for assessing current health status but also for providing clear benchmarks for future health goals.
Integrating Lifestyle Changes
Integrating lifestyle changes based on body composition analysis is fundamental in managing diabetes effectively. To achieve optimal body composition, patients are encouraged to adopt a multifaceted approach that involves both dietary adjustments and regular physical activity. Nutritional guidelines should emphasize a balanced diet that is rich in whole foods while minimizing refined sugars and unhealthy fats. Such dietary changes can facilitate weight loss, improving insulin sensitivity in individuals with diabetes. Additionally, incorporating regular physical activity is critical. Exercise not only aids in fat loss but also promotes muscle gain, thus positively influencing glucose regulation. Research consistently supports the notion that a combination of aerobic and resistance training yields better outcomes in both weight management and metabolic health. Patients can be guided to create achievable exercise routines based on their preferences. As they gradually integrate these lifestyle modifications, the results from body composition assessments can serve as benchmarks for progress. This continuous motivational feedback boosts adherence to lifestyle changes, reinforcing the importance of maintaining a healthy body composition for diabetes management. Ultimately, these efforts can result in significant improvements in overall well-being and a reduction in diabetes-related complications.
Furthermore, it is necessary to recognize the psychological aspects that accompany body composition changes in diabetes management. Achieving and maintaining healthy body composition can be a challenging endeavor, potentially leading to body image issues or feelings of frustration. As individuals embark on their journey toward better health, they might encounter emotional barriers that hinder progress. Therefore, integrating mental health support into diabetes management strategies is essential. Counseling sessions or support groups can provide a safe space for individuals to share experiences and challenges. Emotional support can empower patients to persist through difficulties as they strive for their health goals. It is also beneficial to encourage a focus on overall wellness rather than solely on weight. By highlighting improvements in energy levels, mood, and physical capabilities, patients can cultivate a healthier perspective on their progress. Moreover, recognizing small achievements can motivate continued effort. Encouragement from healthcare professionals plays a critical role in this journey. Engaging patients in discussions about the significance of mindset shifts can reinforce the notion that maintaining a healthy lifestyle is a continuous process driven by long-term benefits rather than immediate aesthetic outcomes.
Monitoring and Continuous Assessment
Another key aspect of effective diabetes management through body composition analysis is ongoing monitoring and assessment. Regular check-ups utilizing the same methods to evaluate body composition create consistency that is essential for tracking progress. This practice allows healthcare providers to detect fluctuations that may indicate underlying issues requiring attention. Early notification of unwanted changes in body composition can facilitate timely interventions, ensuring maintainable health outcomes. Furthermore, it’s important for patients to understand that body composition is not static. Various factors such as age, hormonal changes, and medication can impact body composition. Therefore, tailoring the frequency of assessments based on individual patient needs is vital. Enhanced technologies now offer options such as apps or wearable devices that can provide users with ongoing insights. These modern solutions allow for tracking progress in real time and help to reinforce accountability. Patients should be encouraged to actively participate in their own monitoring process, fostering a sense of ownership over their health journey. Overall, the synergy between continuous assessment and proactive changes in lifestyle practices ultimately supports successful diabetes management.
Medical professionals should also recognize the role of education in conjunction with body composition analysis. Patient education empowers individuals with the knowledge needed to make informed decisions concerning their health. By providing detailed understanding about the significance of body composition, healthcare providers can motivate patients to engage with the analysis process actively. This education can encompass various aspects such as understanding how body fat affects insulin sensitivity and overall metabolic health. Workshops, informational materials, or digital platforms can serve as resources for patients, enhancing their grasp of why monitoring body composition is essential. Furthermore, fostering critical thinking concerning food choices and exercise options can facilitate better behavior patterns. When patients grasp the link between their lifestyle habits and body composition, they are more likely to embrace necessary changes. Continuous education and engagement create an environment that encourages active participation from patients. In turn, this can lead to improved health outcomes. Moreover, by reinforcing this knowledge regularly, healthcare providers can help patients keep their health priorities at the forefront of their daily routines. Patient-centered care promotes greater effectiveness in managing diabetes and contributes to lasting health improvements.
Conclusion and Future Directions
In conclusion, understanding body composition analysis as part of diabetes management offers a comprehensive approach to overall health improvement. This analysis not only aids in identifying risk factors but also serves as a foundation for personalized health strategies. As individuals work towards healthy body composition, they can benefit from tailored exercise and diet plans that actively engage their participation. Moreover, addressing the psychological components associated with body changes fosters a positive experience that fuels motivation. Future advancements in technology are likely to enhance methods of body composition analysis, making them more accessible to patients. Greater emphasis on integrative care approaches combining physical, nutritional, and mental health support can yield significant long-term benefits. The roles of continuous monitoring and patient education will be pivotal in ensuring that individuals find success in managing their diabetes. By fostering a proactive and informed patient population, we can ultimately contribute to a decrease in diabetes-related complications. The journey toward effective diabetes management through body composition analysis is dynamic and focused on individual needs, aiming for a healthier future for all.
As the field of diabetes management evolves, ongoing research is expected to refine body composition analysis methods. Understanding the interplay between body composition changes and diabetes outcomes will continue to enhance available interventions. Ongoing studies will likely lead to more effective tools and technologies for measuring body composition. As these advances develop, they can empower patients further by providing precise feedback on their health status. Moreover, interdisciplinary collaboration between specialists, including nutritionists and exercise physiologists, can lead to enriched diabetes management approaches. Integrating diverse perspectives will ensure that all aspects of body composition are considered holistically. Continuous education and support frameworks will be pivotal in guiding patients through their health journeys. By enhancing body composition insight, individuals may find that diabetes management involves less struggle, paving the way for a more enjoyable experience. As we look to the future, the notion of healthcare being patient-centered will become increasingly necessary. Emphasizing the relevance of body composition helps to reshape conversations around diabetes care. Ultimately, collectively forging paths towards improved health outcomes is the shared responsibility of patients, healthcare providers, and researchers alike.